The Invisible War Within: When Our Own Soldiers Become the Enemy
We're told our immune system is our shield, a vigilant army fighting off invaders. But what if it’s being tricked? New research from India is shining a stark light on a chilling phenomenon: breast cancer cells aren't just a threat to our bodies; they can actively turn our own immune cells against us. This isn't a sci-fi plot; it's a deeply concerning reality where the very mechanisms designed to protect us are being co-opted to help the cancer spread and survive. This investigation dives into the unsettling findings, asking crucial questions about how this betrayal happens and what it means for millions fighting this disease.
The Shifting Loyalties: How Cancer Rewrites the Rules
At the heart of this revelation is the concept of tumour-associated macrophages (TAMs). Imagine your immune system has different types of soldiers. Some are frontline attackers, ready to charge and destroy threats – these are akin to M1 macrophages. They trigger inflammation, a crucial part of the immune response that signals danger and mobilizes defenses to eliminate abnormal cells. However, in the complex battlefield of breast cancer, something insidious happens.
Read More: New Papers Show Epstein Had Health Problems with Sex Hormones
Breast cancer cells, rather than being solely targets, exert a powerful influence on these immune cells. They "push" macrophages into a different state, known as the M2 macrophage. This isn't a minor shift; it's a fundamental reprogramming.
M1 Macrophages: Actively fight tumors, trigger inflammation, and signal for destruction.
M2 Macrophages: Suppress the immune response, promote tumor growth, and help cancer cells evade detection.
The new review by Indian researchers highlights that these M2 TAMs become complicit in the cancer's escape. Instead of recognizing and attacking the malignant cells, they actively suppress other crucial immune cells, particularly T cells. T cells are the sharpshooters of our immune system, capable of identifying and eliminating cancerous cells. By turning these T cells off, the M2 TAMs create a "blind spot" for the cancer, allowing it to grow unchecked, spread to new areas (metastasize), and essentially hide in plain sight from the body's natural defenses.
Read More: AI Finds Sperm, Skin Cells Made Into Eggs for Fertility Help
The core finding is that breast cancer cells manipulate immune cells (macrophages) into an M2 state, which then actively hinders the immune system's ability to fight the cancer, facilitating tumor growth and spread.

This raises a cascade of critical questions:
How precisely do breast cancer cells exert this control over macrophages? What are the specific "commands" they issue?
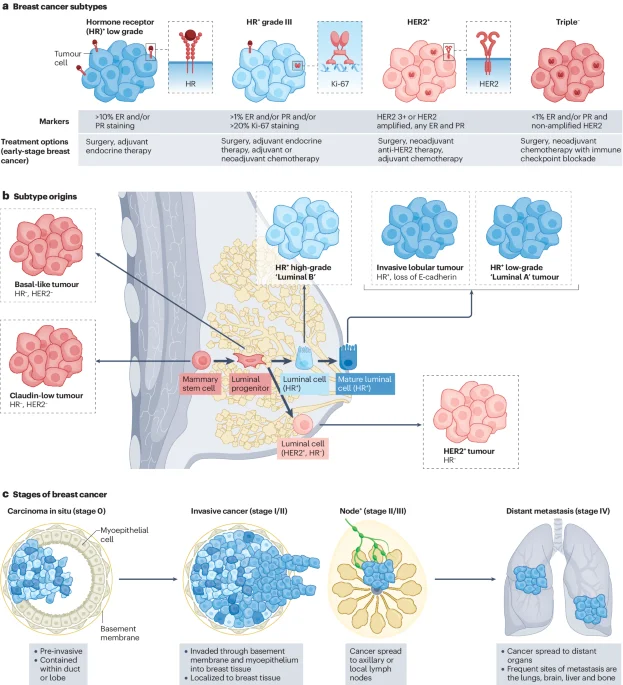
Is this M2 reprogramming a universal feature of all breast cancers, or are there subtypes that are more adept at this immune subversion?
What are the earliest signs of this immune "betrayal" within the tumor microenvironment?
Beyond the Tumor Cell: The Invisible Microenvironment
For a long time, much of the focus in understanding cancer has been on the tumor cells themselves – their mutations, their rapid division, their invasive capabilities. While these are undeniably critical, the groundbreaking work emphasizes that the battleground extends far beyond the cancer cells' own DNA. The tumor microenvironment, the complex ecosystem surrounding the tumor, is a crucial player.
Read More: Actor James Van Der Beek Dies at 48 from Bowel Cancer; Early Signs Often Missed
This environment is not inert; it's a bustling hub of interactions between cancer cells, immune cells, blood vessels, and structural proteins. The Indian researchers' work zeroes in on how cancer hijacks the immune component of this microenvironment.
Historically, our understanding of immune cells in cancer has often painted them as either allies or antagonists. However, this new perspective reveals a more nuanced and disturbing reality: immune cells can switch sides.
"Within tumours, these cells often change their behaviour and become tumour-associated macrophages (TAMs)—immune cells that now work in favour of the cancer rather than against it."
This statement from the article is powerful. It suggests a dynamic, adaptive enemy that can weaponize our own biological processes.
Past Incidents: While the current study is new, the concept of immune cells being manipulated in cancer isn't entirely novel. Researchers have long observed that the tumor microenvironment can be immunosuppressive. However, the specific focus on macrophages being reprogrammed to actively suppress T cells and aid metastasis is a significant step forward in understanding the mechanism.
Previous Research: Studies on various cancers have noted the presence of M2 macrophages and their correlation with poor prognosis. The review cited in Article 6 ("Towards targeting the breast cancer immune microenvironment") likely delves into these broader interactions within the breast cancer ecosystem.
Read More: New Ways to Help People Have Babies Using Science
The tumor microenvironment is not just a passive setting but an active participant where cancer cells strategically reprogram immune cells to aid their survival and spread.

This begs further questions:
What are the key signals exchanged between breast cancer cells and macrophages that trigger this M2 transformation?
Are there specific genetic mutations in breast cancer cells that are more likely to induce this immunosuppressive M2 state?
How does this M2 reprogramming impact the effectiveness of existing immunotherapies, which rely on a robust T cell response?
The Double-Edged Sword: Inflammation and Its Paradoxical Role
Inflammation is a classic immune response, typically associated with fighting off pathogens and repairing tissue. As we've seen, M1 macrophages are pro-inflammatory and anti-tumorigenic, while M2 macrophages are anti-inflammatory and pro-tumorigenic. This research highlights how breast cancer exploits this delicate balance.
Read More: Know the Early Signs of Colon Cancer
The cancer cells don't just passively benefit from the M2 state; they actively create conditions that favor it. This is where things get even more complex. The development of an acidic environment within cancer cells, for instance, has been linked to the release of lactic acid. Article 3, discussing research from the Indian Institute of Science (IISc), notes that Interferon-gamma (IFN-γ) treatment in some cancer cells led to an acidic environment due to lactic acid release, potentially indicating resistance to immunotherapy. This acidic milieu could be a signal that encourages the M2 reprogramming of macrophages, making the tumor environment more hospitable for the cancer.
| Macrophage Type | Primary Role in Cancer Context | Effect on Immune System | Pro-Tumorigenic/Anti-Tumorigenic |
|---|---|---|---|
| M1 | Attack tumor cells, initiate inflammation | Activates T cells, alerts immune system | Anti-Tumorigenic |
| M2 | Suppress immune response, promote tissue repair/remodeling, aid angiogenesis | Inhibits T cells, dampens immune surveillance | Pro-Tumorigenic |
Read More: Drinking Coffee and Tea May Lower Risk of Dementia
Metabolic Shifts: Cancer cells undergo significant metabolic changes to fuel their rapid growth. This includes altered glucose metabolism, leading to increased lactic acid production. Is this metabolic shift a deliberate strategy to create an M2-favoring environment?
Therapeutic Implications: If acidity and lactic acid production are key enablers of M2 TAMs, could therapies targeting these metabolic pathways offer a new avenue to disrupt cancer's immune evasion?
Breast cancer cells actively create metabolic and chemical cues, such as acidity from lactic acid, that likely promote the M2 macrophage state, thus furthering immune suppression.
This leads us to ask:
Are there specific biochemical pathways breast cancer cells utilize to induce the M2 state in macrophages?
Can we measure the levels of lactic acid or other metabolites in the tumor microenvironment as a diagnostic or prognostic indicator?
Towards a Counter-Offensive: Enhancing Immunity Against Cancer
Understanding how cancer subverts our immune system is the first step; the next is finding ways to reverse it or bolster our defenses. The research from Indian scientists, including the work on enhancing immunotherapy (Article 3), points towards potential strategies.
Read More: New Way Cells Talk in Tumors Found
The IISc study highlighted the role of Interferon-gamma (IFN-γ). While it seemed to induce an acidic environment in some cancer cells, suggesting potential resistance, the fundamental role of IFN-γ is to boost immune responses. This hints at a complex interplay: certain treatments might have dual effects, and understanding these nuances is critical.
Beyond direct therapeutic interventions, there's a growing interest in natural modulators of immunity. Reviews exploring the effects of nature exposure on the immune system (Article 2) and the role of Ayurvedic medicine (Article 5) suggest that external factors can influence immune function. While these are broad areas, they raise the question: could lifestyle or natural interventions potentially support the immune system in ways that make it less susceptible to cancer's manipulation?
Synergistic Therapies: Could combining existing immunotherapies with agents that prevent macrophage reprogramming or boost T cell activity offer a more potent attack against cancer?
Early Detection: Can we develop biomarkers to detect the M2 macrophage shift early in breast cancer, allowing for more timely and targeted interventions?
Natural Approaches: While not a direct treatment, how do factors like diet (mentioned in Article 4) and a healthy lifestyle potentially contribute to a robust immune system that is better equipped to resist cancer's subversion tactics?
The path forward likely involves not just directly attacking cancer cells but also actively restoring or enhancing the immune system's ability to recognize and combat cancer, potentially through targeted therapies and understanding natural immune boosters.
This complex research prompts vital questions for the future of cancer treatment:
What are the most effective strategies for "re-educating" M2 macrophages back into an anti-tumor M1 state, or eliminating them entirely?
How can we translate the understanding of the tumor microenvironment's role in immune evasion into clinically actionable treatments for breast cancer patients?
What is the precise balance between boosting immune responses and avoiding potential detrimental effects, as suggested by the IFN-γ example?
The Unseen Battlefield: A Call for Deeper Investigation
The findings from Indian researchers are a stark reminder that cancer is not a static foe. It's an evolving adversary that learns, adapts, and, most alarmingly, manipulates our body's own defense mechanisms. The reprogramming of immune cells into TAMs, particularly the M2 subtype, represents a sophisticated evasion strategy that turns our natural allies into unwitting collaborators of tumor growth and metastasis.
This necessitates a paradigm shift in how we approach breast cancer research and treatment. While understanding tumor cell biology remains crucial, the intricate dance within the tumor microenvironment, especially the betrayal orchestrated by immune cells, demands equal, if not greater, attention.
Moving forward, the critical next steps involve:
Detailed Mechanistic Studies: Elucidating the precise molecular pathways through which cancer cells induce M2 polarization in macrophages.
Therapeutic Development: Designing drugs or therapies that can specifically target M2 macrophages, inhibit their immunosuppressive functions, or reverse their polarization.
Biomarker Discovery: Identifying reliable markers in the blood or tumor tissue that can indicate the presence and activity of immunosuppressive TAMs, enabling early intervention.
Clinical Trials: Rigorously testing novel therapeutic strategies that target the tumor immune microenvironment in breast cancer patients.
The battle against breast cancer is being fought not just on the cellular level of tumor growth but also on the complex immunological battlefield within our bodies. Understanding and countering this immune betrayal is paramount to developing more effective treatments and, ultimately, saving lives.
Sources:
The Hindu: Review by Indian researchers notes that body’s immune cells ‘betray’ it to help breast cancer spread. https://www.thehindu.com/sci-tech/health/study-by-indian-researchers-finds-that-bodys-immune-cells-betray-it-to-help-breast-cancer-spread/article70594578.ece
PubMed (Review): Nature Exposure and Its Effects on Immune System Functioning: A Systematic Review. https://pmc.ncbi.nlm.nih.gov/articles/PMC7913501/ (Note: This is a general review; direct relevance to cancer subversion is indirect.)
India Today: Indian researchers reveal key to enhancing immunity against cancer. https://www.indiatoday.in/science/story/indian-researchers-reveals-key-to-enhancing-immune-cells-defense-against-cancer-2475017-2023-12-12
PubMed (Review): Common foods for boosting human immunity: A review. https://pubmed.ncbi.nlm.nih.gov/37970422/ (Note: General review on immunity.)
PubMed (Review): Nature and mechanism of immune boosting by Ayurvedic medicine: A systematic review of randomized controlled trials. https://pubmed.ncbi.nlm.nih.gov/35721243/ (Note: General review on immune boosting.)
Nature Reviews Cancer: Towards targeting the breast cancer immune microenvironment. https://www.nature.com/articles/s41568-024-00714-6
ScienceDirect: Human immune system: Exploring diversity across individuals and populations. (Low Priority - Extraction failed/content too short)
ScienceDirect: Phytoimmunomodulators: A review of natural modulators for complex immune system. (Low Priority - Extraction failed/content too short)






:max_bytes(150000):strip_icc()/VWH_EarlySignsofColonCancer-be7dc99d4bfb4a37b2e6bec8d9f4cfd7.png)

