The financial health of healthcare organizations hinges on effective Revenue Cycle Management (RCM). As the sector navigates evolving patient expectations, regulatory shifts, and technological advancements, RCM strategies are adapting. The focus is shifting towards a more integrated, patient-centric, and technology-driven approach to manage the entire financial lifecycle of patient care, from initial scheduling to final payment. This report examines the prominent trends and critical metrics shaping RCM in 2026.
Evolving Landscape of Healthcare Finance
Healthcare providers face increasing financial pressures. These pressures stem from a combination of factors:
Changing regulations impacting reimbursement and compliance.
Rising patient expectations for transparency and convenience in financial matters.
The need for improved cash flow and reduced administrative burdens.
A growing emphasis on patient experience as a driver of financial performance.
Key Trends Shaping RCM in 2026
Several overarching trends are directing the evolution of RCM practices.

Patient-Centric Financial Experiences
A significant shift is occurring in how healthcare organizations approach patient finances.
Patient experience and financial performance are increasingly linked. Organizations are recognizing that a positive patient financial journey can lead to better satisfaction, faster payments, and greater loyalty.
This involves enhancing patient-centered billing and offering patient self-service tools.
Transparency in pricing and financial responsibilities is becoming paramount.
Integration and Technology Adoption
The integration of various healthcare systems and the adoption of new technologies are central to modern RCM.
Swift integration between Electronic Health Records (EHRs), practice management systems, and billing platforms is emerging. This aims to create more cohesive workflows and improve data exchange.
Artificial Intelligence (AI) and automation are being explored, though the idea of "end-to-end RCM automation" is viewed as unrealistic.
The practical path forward appears to be selective, stage-wise AI augmentation rather than full automation.
Cybersecurity and Data Integrity
The proliferation of digital health services magnifies the importance of cybersecurity.
Read More: Healthcare Practices 2026: Key Financial Metrics to Track for Better Collections
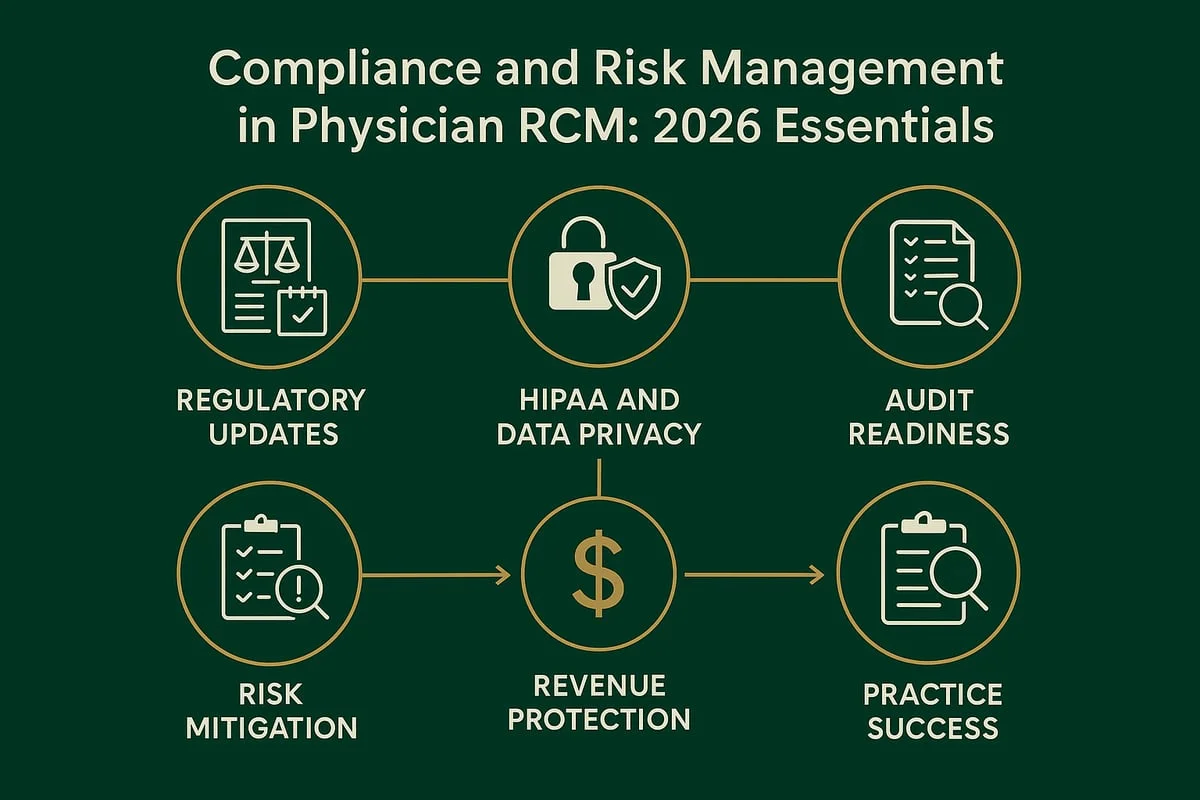
Cyber incidents are increasingly viewed as revenue incidents. Protecting sensitive financial and patient data is crucial to prevent revenue loss and maintain trust.
Practices must implement robust cybersecurity measures and ensure regulatory compliance.
Strategic Partnerships and Outsourcing
The complexity of the RCM process is driving a move towards more strategic partnerships.
Many organizations are considering outsourcing their RCM needs. This often involves seeking end-to-end RCM partners who manage front-end access, mid-cycle integrity, and back-end collections.
When outsourcing, providers are advised to vet partners for cybersecurity, regulatory compliance, and technological capabilities.
Interoperability and Data Exchange
Seamless data exchange remains a critical, albeit sometimes challenging, aspect of RCM.
Interoperability inefficiencies can stall patient care, financial performance, and data-driven decisions. Enhancing data exchange across systems is vital for improved patient care coordination and efficient RCM.
Essential RCM Metrics for 2026
Tracking key performance indicators (KPIs) is vital for understanding and optimizing RCM processes. While specific metrics may vary, several are consistently highlighted.
| Metric | Description | Why It Matters |
|---|---|---|
| Net Collection Rate (NCR) | Percentage of payments collected from the total amount allowed, per insurance contracts. | Measures the ability to collect revenue based on contracted rates. |
| Gross Collection Rate (GCR) | Percentage of gross charges collected. | Provides a snapshot of overall collection effectiveness before adjustments. |
| Unbilled Claims Percentage | Percentage of claims not yet billed out against average daily claims volume. | Indicates delays in the billing process, impacting cash flow. |
| Days in Accounts Receivable (AR) | The average number of days it takes to collect payment after a service is rendered. | Measures the efficiency of the collections process. |
| Clean Claim Rate | Percentage of claims submitted without errors that require re-submission. | Reflects the accuracy of data entry and coding, directly impacting denial rates. |
| Denial Rate | Percentage of claims rejected by payers. | Highlights issues in the initial claim submission process, leading to revenue loss. |
| Cost to Collect | The cost incurred to collect payments. | Helps assess the efficiency of revenue cycle operations. |
| Average Revenue per Encounter (ARE) | The average amount of revenue collected per patient encounter. | Offers insight into the overall revenue generated per patient visit. |
It is crucial to establish benchmarks for these metrics to accurately gauge performance and identify areas for improvement.
Expert Analysis
The integration of AI and automation in RCM is seen not as a complete replacement for human processes, but as a way to augment them.
"The practical path forward is selective, stage-wise AI augmentation, not full automation." - Boston Technology Corporation
Furthermore, the emphasis on patient experience is a recurring theme:
"Patient experience and financial performance can no longer be viewed separately." - Nyx Med
The interconnectedness of different RCM functions is also stressed:
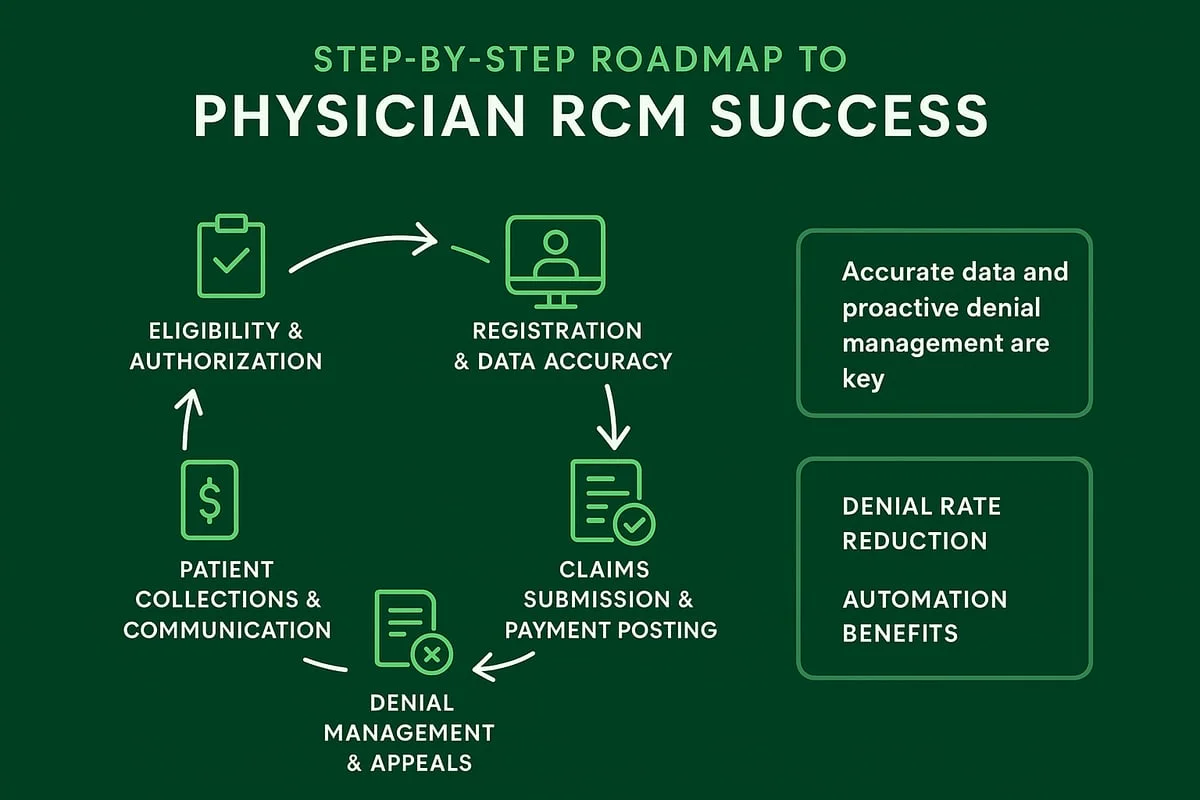
"The front end of your revenue cycle determines the success of the back end." - PHIMED Technologies
Conclusion and Implications
Revenue Cycle Management in 2026 is characterized by a strategic evolution towards greater patient engagement, technological integration, and robust data management. The trend lines indicate a move away from purely transactional processes towards a more holistic approach that values patient satisfaction alongside financial outcomes.
Read More: US SEC Drops Crypto Cases, Making Rules Clearer for Digital Assets in 2025
Key takeaways include:
The patient financial experience is a critical component of overall RCM success.
AI and automation are tools for augmentation, not wholesale replacement.
Cybersecurity is inextricably linked to revenue integrity.
Interoperability and seamless data exchange remain foundational for efficient RCM.
Healthcare organizations that prioritize these trends and diligently track relevant metrics will be better positioned to navigate the complexities of the healthcare financial landscape, ensuring both operational efficiency and long-term financial sustainability. The need for adaptability, continuous process improvement, and strategic partnerships will remain paramount.
Sources Used:
Nyx Med: https://nyx-med.com/2026/01/03/key-rcm-trends-to-watch-in-2026/
Plutus Health Inc.: https://www.plutushealthinc.com/post/revenue-cycle-management-kpi
AGS Health: https://www.agshealth.com/blog/four-rcm-trends-for-healthcare-leaders-to-watch-in-2026/
Boston Technology Corporation: https://www.boston-technology.com/blog/end-to-end-rcm-automation-is-a-myth-4-step-realistic-ai-roadmap-for-2026
DrCatalyst: https://www.drcatalyst.com/blog/revenue-cycle-management-trends
RCM Workshop: https://rcmworkshop.com/insights/blogs/future-proofing-your-revenue-cycle-trends-to-watch-in-2026/
PharmBills: https://pharmbills.com/blog/the-future-of-rcm-revenue-cycle-management-trends-to-watch
PHIMED Technologies: https://phimed.com/2025/12/2026-rcm/
ADSC: https://www.adsc.com/blog/rcm-revenue-cycle-management-everything-healthcare-providers-need-to-know-1
Greenhive Billing Solutions: https://greenhivebilling.com/physician-rcm/
Alpine Pro Health: https://alpineprohealth.com/blog/rcm-trends-2026-strategic-insights-for-healthcare-leaders/
Practolytics: https://practolytics.com/blog/key-metrics-every-practice-should-track-for-revenue-cycle-management-success/
Unislink: https://unislink.com/rcm-best-practices-blog/seven-most-important-rcm-metrics-for-every-medical-practice/
Dean Dorton: https://deandorton.com/rcm-healthcare-metrics/







